Hi fellow CMIOs, CNIOs, and other Applied Clinical Informatics and #HealthIT friends,
Today I thought I'd share the first ten (of 20) strong suggestions I put together into slides for other Applied Clinical Informaticists, or those considering a career in Applied Clinical Informatics. I'm hoping this helps shed light on the importance and value of this role in modern healthcare, and how it helps to evaluate, implement, and maintain clinical technology and content.
First, my #1 advice to newcomers - Always map the CURRENT-STATE and FUTURE-STATE workflows. While some might argue this is an unnecessary step, this exercise will benefit you in some very important ways :
- It will help you understand and relate to your end-users.
- It will help you determine just how much work it takes to get from your CURRENT STATE (Point A) to your FUTURE STATE (Point B), which is necessary to help plan and allocate resources.
- Finally, it will help you develop blueprints, develop downtime forms, identify stakeholders, and scope/prioritize your projects.
Next, for my strong recommendation #2, I'd like to share how to write a good task, and then a good procedure. Learning to write a good task and procedure are so instrumental in building or untangling workflows, that it can even be used as a quick substitute for swimlane diagrams (e.g. when trying to quickly document a workflow during a video chat with clinical end-users) :
Strong recommendation #3 involves something that sounds dull, until you learn about how it impacts your infrastructure and operations - Document management. Learning how to create, edit, and archive documents can actually be a very powerful way of shaping or augmenting workflows in your electronic medical record. My mantra for newcomers : "Learn to control your documents, before they control you."
My next strong recommendation #4 is to learn the basic structure of healthcare operations, by understanding the relationship between Administrative, Academic, Research, and Clinical Enterprises (Note : Smaller community hospitals typically only have Academic and Clinical enterprises.) In short : Administration supports the needs of the Academic, Research, and Clinical Enterprises. Learning how to navigate the people in these areas will help you break down silos, untangle workflows, and improve collaboration.
Coming in at #5 is my strong recommendation to care about hard work, details, and precision. "In Healthcare, there are no shortcuts." While timelines are often short, and there is often pressure to move ahead, try to resist the temptation to serve workflows that are not complete. (They may get you across your project finish line, but you risk having to do the whole project again, especially if end-users are not satisfied with the results.)
Strong Recommendation #6 might be a surprise to some : When working in a team, file naming conventions really matter. Group files should be both easy-to-find and easy-to-identify. My own personal favorite is :
DRAFT/FINAL - ARCHETYPE - Descriptor - Created/Updated/Approved mm-dd-yyyy.ext
Where :
- DRAFT / FINAL = Use DRAFT for documents in development, FINAL when approved
- ARCHETYPE = Describes the file type (e.g. Education, Budget, Order Set, Catalog, Index, Contract, Policy, Protocol, Guideline, Schedule, Bylaws, Notes, Slide, Screenshot, etc.)
- Descriptor = Describes a unique identifier for the file (e.g. "ICU DKA Treatment Discussion", "Meeting with Dr. Smith", "Malaria Workup", etc.)
- Created/Updated/Approved = Use CREATED when first creating a file, UPDATED when updating a file, and APPROVED when creating a final version
- mm-dd-yyyy = Describes when the file was created, updated, or approved
- ext = File extension (e.g. ".docx" or ".PDF", etc.)
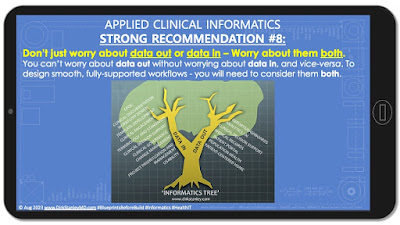
Coming in at #8 is my general recommendation to all Applied Clinical Informaticists to care about the entire 'Informatics tree', including both the 'Data In' and 'Data Out' branches. While most people will gravitate toward one area, understanding the whole tree will broaden your perspectives and skill sets, and overall help you plan workflows :
Strong Recommendation #9 for Applied Clinical Informaticists seeking to design smooth workflows comes from this 2015 blog post, where I recommend learning the relationship between concepts, terminology, templates, documents, and workflows. In general :
- Organizational Support (#8) is necessary to...
- identify the concepts and ontologies (#7) that help you...
- develop the definitions, terminology, and standards (#6) that you need to...
- develop the templates and archetypes (#5) that will help you...
- create the documents and tools (#4) that, combined, will help to...
- create and support the workflows and processes (#3) that, if designed properly, will...
- align with your goals and regulations (#2) which should...
- align with your Mission and Vision (#1).
Typically, after first understanding #2, Applied Clinical Informaticists will concern themselves with aligning levels #7-#3 of this pyramid. (Learning how pyramid levels #8-5 impact the documents in #4 can help you troubleshoot even the most complicated workflows in #3.)
Finally, my Strong Recommendation #10 for Applied Clinical Informaticists seeking to design smooth workflow is to care deeply about change management. While Kotter's 8-step change management model is an excellent foundation, I recommend beginning with a standard, linear waterfall project model and then expanding it slightly for healthcare purposes, to include :
- Conception, Determination, and Documentation of Need for Change
- Evaluation, Analysis, Scoping, Presentation, Prioritization, and Approval for Change
- Project Planning
- Drafting of Change
- Building of Change
- Testing of Change
- Final Approval of Change (go / no-go discussion)
- Communication and Education of Change
- Implication / Publication ('Go-Live') of Change
- Monitoring and Support of Change
Once you have these ten steps laid out, you can begin looking at the tasks beneath each step, and developing your own 'waterfall-meets-healthcare'-type change management strategy.
I hope this is a helpful set of slides for newcomers to Applied Clinical Informatics. Feel free to leave comments below with any thoughts or feedback. In my next post, we will look at another ten (10) of my strong recommendations for Applied Clinical Informaticists seeking to design smooth workflows!
Have any helpful advice for newcomers to Applied Clinical Informatics? Are there any tips or tricks that were important to you? Please feel free to leave in the comments section below!










1 comment:
#6 is SO IMPORTANT! The mistakes I made early in my career, both in my work and academic careers. After you learn better, you do better!
Post a Comment